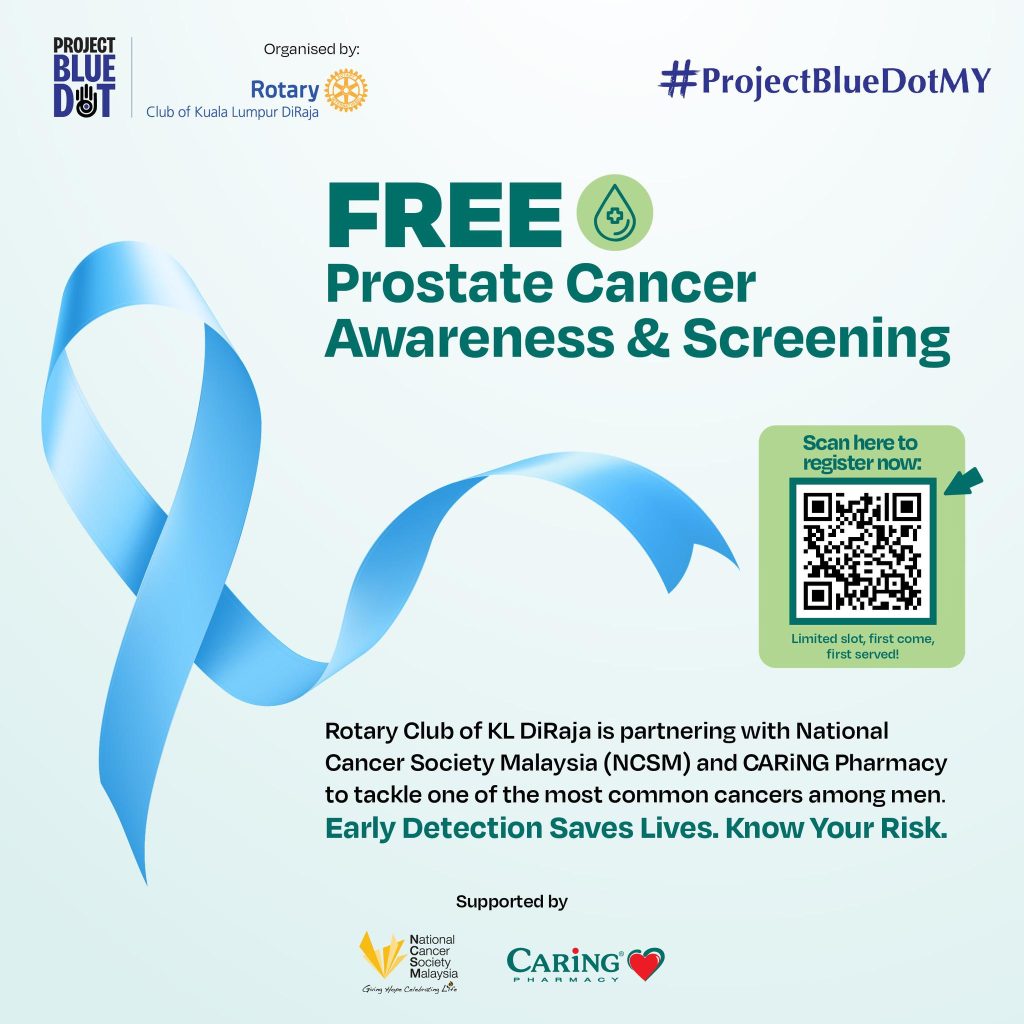
BIG CARiNG Group in collaboration with Rotary Club of Kuala Lumpur DiRaja (RCKL DiRaja) and the National Cancer Society of Malaysia (NCSM) to roll out Project Blue Dot, a nationwide initiative aimed at increasing access to prostate cancer screening and early detection, particularly among B40 and high-risk groups.
As its first major milestone, Project Blue Dot will sponsor 3,000 free Prostate-Specific Antigen (PSA) screenings for B40 Malaysian men aged 45 and above.
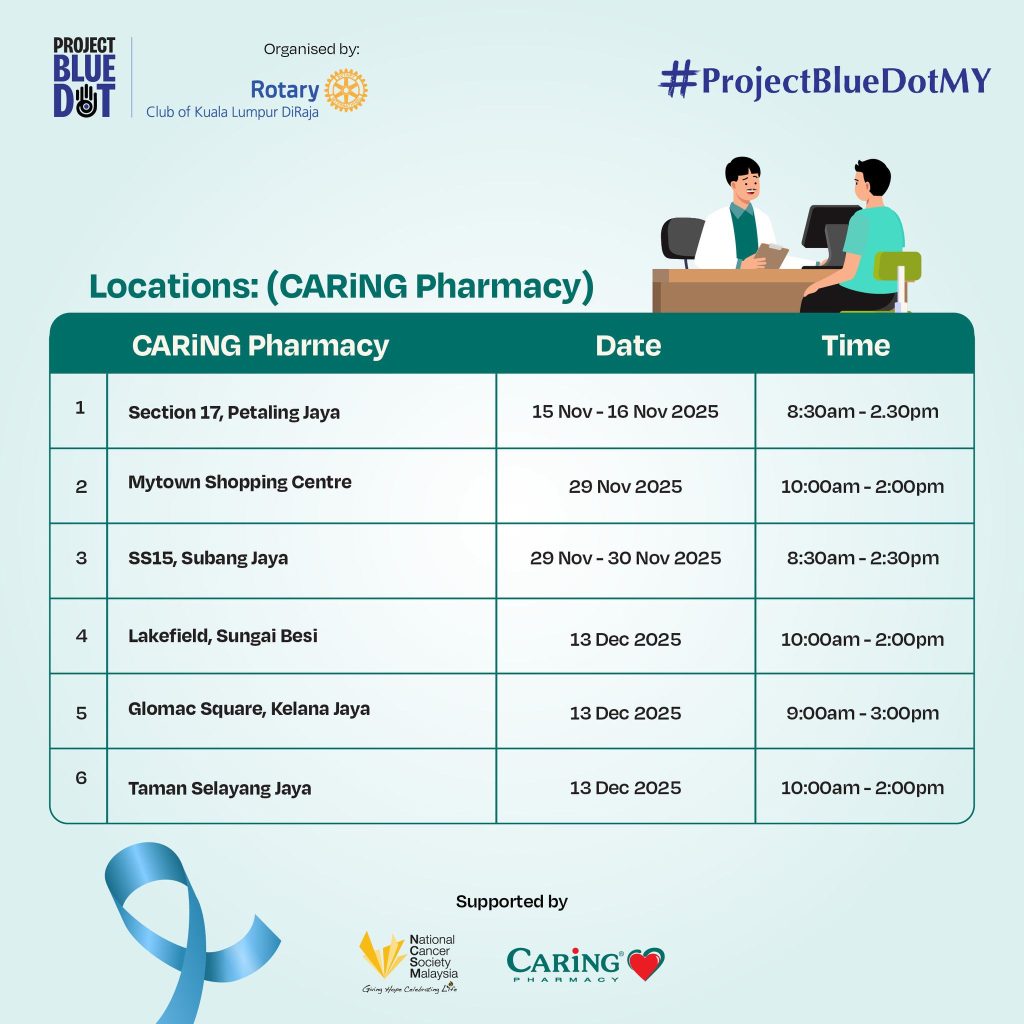
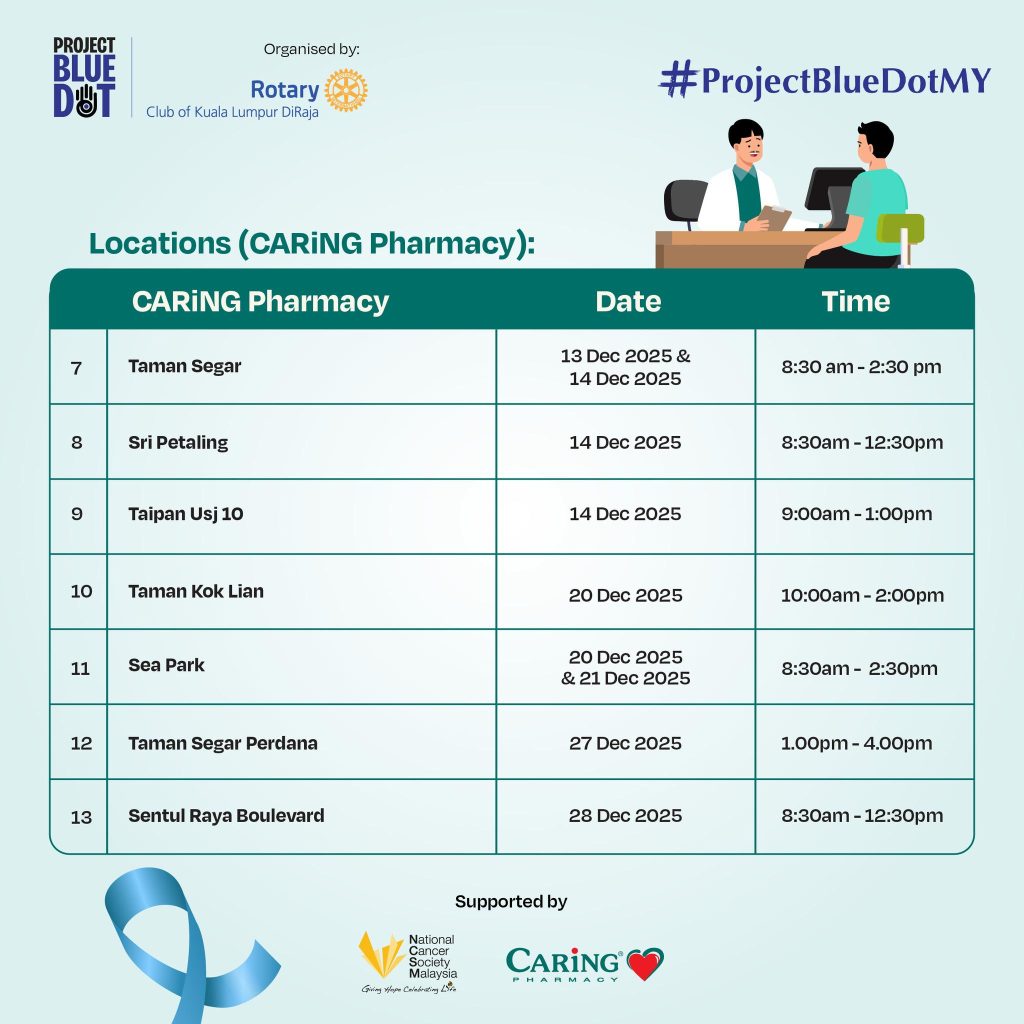
Screenings will be conducted at selected BIG Pharmacy and CARiNG Pharmacy outlets across the Klang Valley from 15 November 2025 to 11 January 2026.
To ensure you can utilise this opportunity provided by our partners, please reserve your slot by scanning the QR code below:
For more information on the locations available: